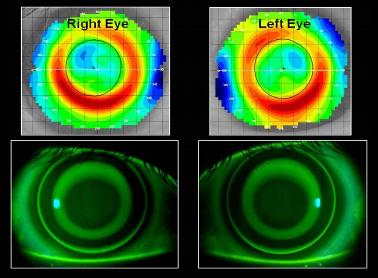
| Column Dry Eyes and Corneal Refractive Therapy Hardly a day goes by without a patient reporting symptoms of dryness when wearing soft contact lenses. In 2005, Nichols et al reported that 52% of contact lens wearers reported having dry eyes at some time throughout their contact lens wearing schedule. This number was found to be 12 times higher than that of emmetropes requiring no ocular correction. Therefore, it is not surprising that the most frequently reported reason for soft lens dissatisfaction and discontinuation is dry eye-related symptoms. So how do we manage our contact lens patients who are unable to obtain adequate comfort and/or wearing time secondary to dryness? Step one is always the same: rule out the possibility of the preserved lens care products as the source of the symptoms. This is often accomplished by switching the patient to daily disposable lenses or initiating a preservative-free disinfection system such as hydrogen peroxide. If the dry eye symptoms continue, you can then begin a regimen of dry eye treatments that may include preservative-free artificial tear therapy, omega-3 supplements, lid hygiene, ocular anti-inflammatory agents and punctual occlusion. However, even with maximum dry eye therapies, some CL patients continue to experience dry eye symptoms. Many of these patients seek to resolve their contact lens failure by pursuing refractive surgery, but patients need to be cautioned that laser surgery can adversely affect tear production and that patients with preexisting dry eyes are at a higher risk of developing significant post-operative dry eye complications. Over the years, we and others have reported some success in successfully managing these patients’ refractive errors with corneal refractive therapy. One such individual is a 28-year-old female with a refractive error of -3.50D sphere in the right eye and -3.75D sphere in her left eye. She had a four-year history of dry eyes with contact lenses despite numerous attempts with a wide range of daily disposable lenses and appropriate dry eye therapies. The patient was free of any corneal or conjunctival pathology, and she reported that her dry eye symptoms were significantly reduced when she wore her spectacle correction. However, she insisted that glasses were not an option for her lifestyle. She was an avid runner and biker and, in the rainy Pacific Northwest of the USA, glasses are a significant problem. Patient’s post-fitting corneal topography and fluorescein photos. It was at that time that we suggested the possibility of contact lens corneal reshaping. Clinical experience has taught us that some dry eye patients do exceptionally well with the overnight reshaping therapy. The closed eye environment may prevent excessive tear evaporation, a contributing cause of dry eye symptoms in some contact lens wearers. With the overnight reshaping modality, many patients report improved daily comfort since no corrective device is on their eyes throughout the day to stress the tear film. The patient was successfully fitted with Paragon CRT lenses, and within seven days her uncorrected visual acuity was a stable 20/20 or 1.0 throughout her waking hours. The patient reported no overnight ocular discomfort with the lenses and no dry eye symptoms throughout the day. We believe that a number of contact lens-induced dry eye patients may be excellent candidates for corneal reshaping. This is especially true for those individuals considering surgical intervention as a refractive treatment. Reference: http://www.iovs.org/content/46/6/1911.abstract |

| Patrick Caroline is an associate professor of optometry at Pacific University and a consultant to Paragon Vision Sciences. |